Atypical BPPV: When Positional Testing Doesn’t Match the Textbook
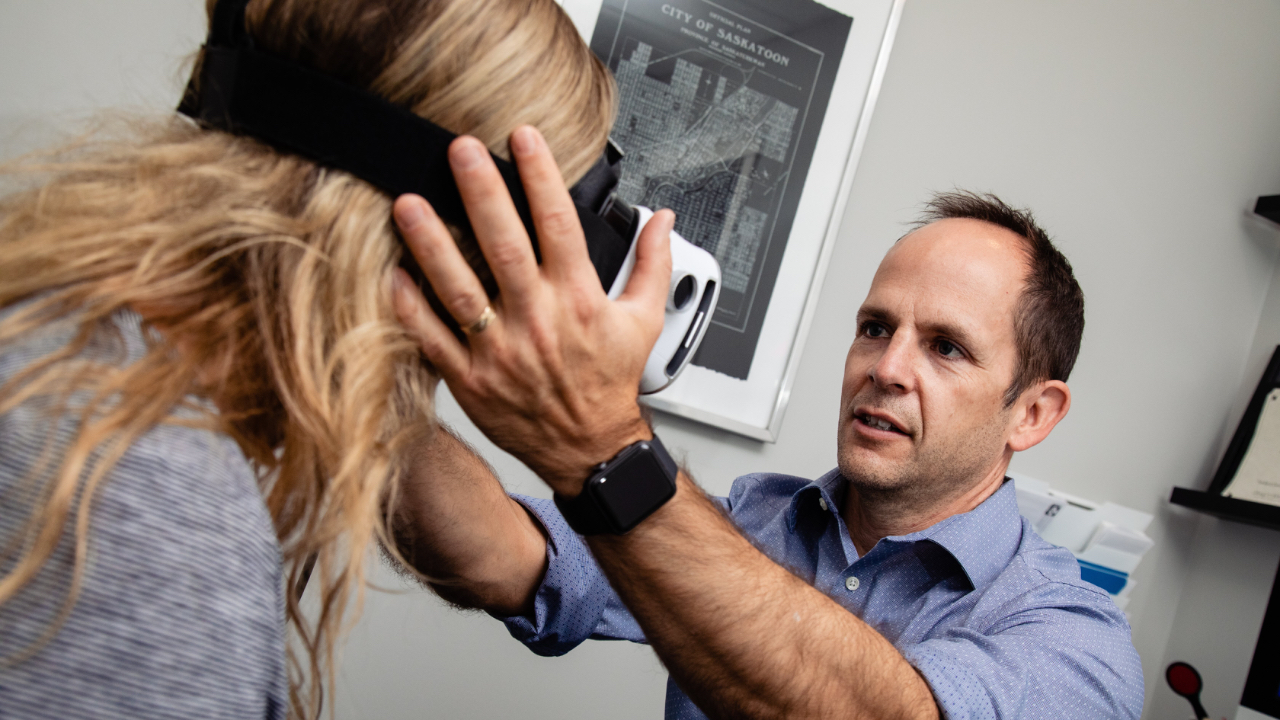
A 1-hour, evidence-based course to help clinicians recognize and manage posterior canal BPPV variants with confidence.
When BPPV Doesn’t Behave the Way You Were Taught
Benign paroxysmal positional vertigo is often taught as one of the most straightforward vestibular diagnoses: take a history, perform a Dix-Hallpike, observe canal-specific nystagmus, apply the appropriate repositioning maneuver, and symptoms resolve.
And most of the time, that’s true ... until it isn’t.
When this happens it is natural to think:
“Am I missing something?”
“Is this still BPPV?”
“Is this central?”
“Do I keep treating, or do I refer?”
“Why isn’t what I was taught working?”
This uncertainty erodes confidence, especially when BPPV is supposed to be the “easy win.”

Why This Happens
(and Why It’s Not Your Fault)
Traditional teaching focuses on typical posterior canal canalithiasis, where otoconia reside in the most dependent portion of the long arm and produce predictable, textbook nystagmus.
However, research and clinical observation now show that a significant proportion of posterior canal BPPV cases are atypical and can include:
-
Short-arm canalithiasis
-
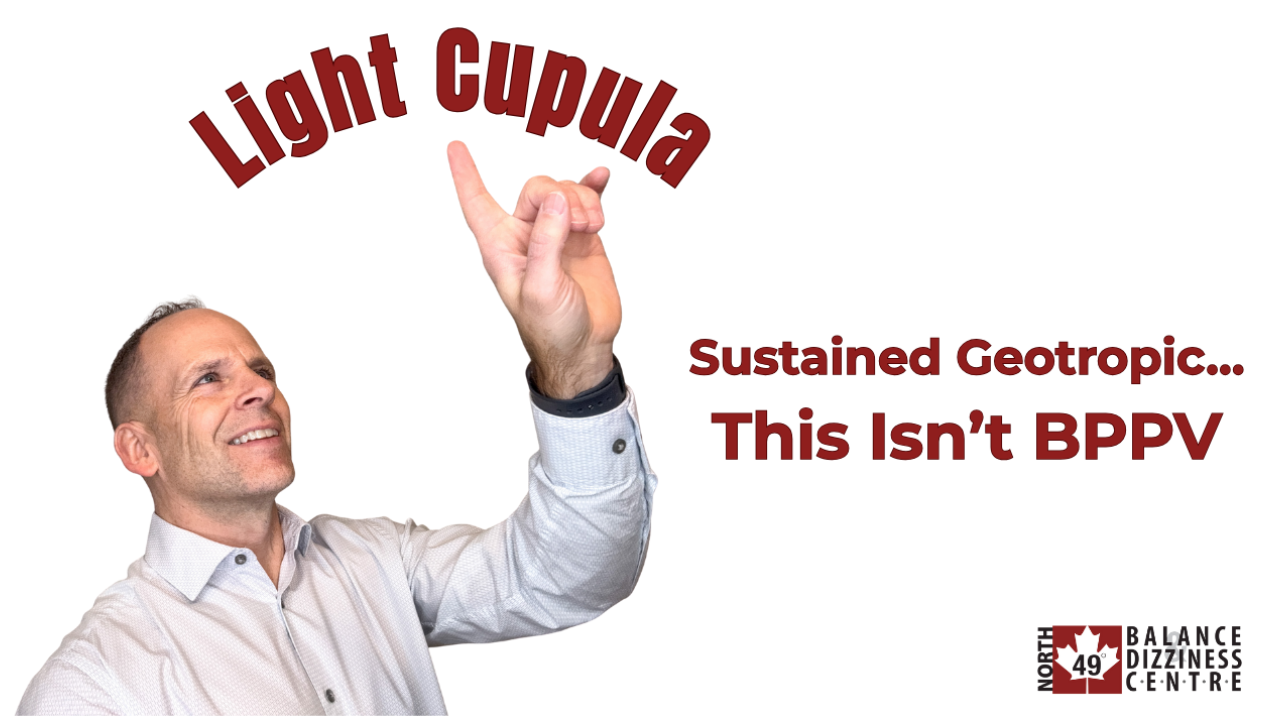
Cupulolithiasis
-
Distal long-arm variants
-
Periampullary canalithiasis
In these cases:
-
The orientation of the cupula relative to gravity may be neutral or near-vertical.
-
Small differences in head extension, anatomy, or otoconial position can completely change the observed response.
The result is variable, misleading, or absent nystagmus—despite a history that still fits BPPV.
This is why:
-
Dix-Hallpike testing can be negative.
-
Nystagmus may only appear on sitting up.
-
Findings may mimic anterior canal BPPV or even central pathology.
-
Standard maneuvers may fail, despite being performed correctly.
What Clinicians Actually Need
What’s missing isn’t effort or experience, it is structure.
Clinicians need:
👉🏻 A way to recognize atypical patterns early
👉🏻 An understanding of why the findings look wrong
👉🏻 Confidence to rule out central causes appropriately
👉🏻 A mechanism-based approach to choosing alternative tests and maneuvers
👉🏻 A clear plan for when the Epley or Semont fails
That is the gap this course is designed to fill.
How This Course Solves the Problem
This 1-hour course focuses on:
👉🏻 Classifying common atypical posterior canal BPPV presentations
👉🏻 Explaining the mechanisms behind confusing findings
👉🏻 Identifying clinical clues that suggest an atypical variant
👉🏻 Selecting targeted, mechanism-specific treatment options
👉🏻 Applying a repeatable framework that restores confidence and improves outcomes
Rather than memorizing exceptions, clinicians learn how to reason through when BPPV does not behave as expected.
Frequently Asked Questions
You’ll have lifetime access to the course, allowing you to revisit the material 24/7.
This 1-hour online course includes:
-
7 on-demand video lessons
-
A structured framework for recognizing atypical posterior canal BPPV
-
3 case studies with vidoe recording of their positional testing results
-
Practical assessment and treatment strategies
- Quick reference handout to access during your busy day
-
A downloadable reference handout
-
A course completion certificate
In this 1-hour course, you’ll learn how to:
-
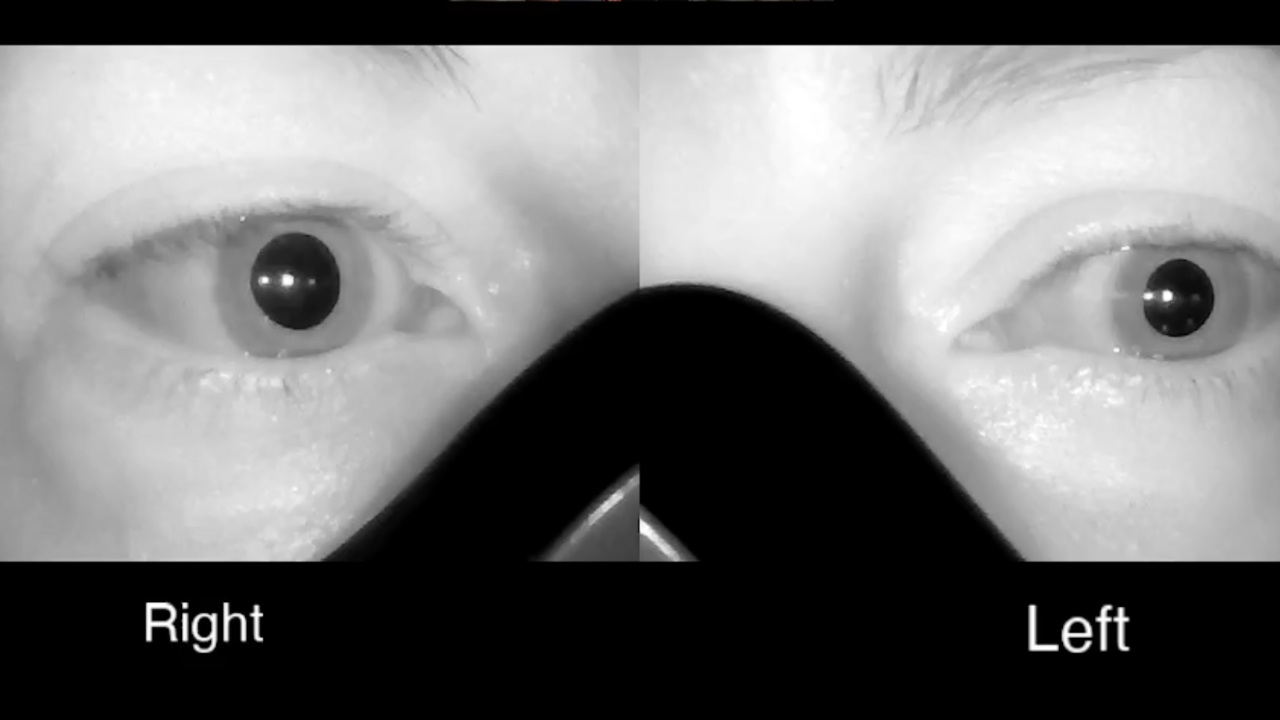
Recognize atypical BPPV presentations with confidence, including cases that present with negative Dix-Hallpike testing, nystagmus on sitting up, or misleading downbeat patterns.
-
Interpret confusing positional test findings correctly, understanding why nystagmus may be absent, reversed, sustained, or appear only during transitions.
-
Apply assessment and treatment techniques specific to atypical posterior canal BPPV, including short-arm canalithiasis, cupulolithiasis, and other variants when traditional maneuvers do not work.
-
Select mechanism-based alternative maneuvers when the modified Epley or Semont fails, rather than repeating techniques without a clear rationale.
What this means clinically:
Instead of second-guessing your diagnosis or wondering whether you’re missing a central cause, you’ll have a clear framework for understanding why findings look the way they do and what to do next. This allows you to approach atypical BPPV cases with greater confidence, efficiency, and reassurance for both you and your patients.
This course is designed for licensed healthcare professionals who assess and treat patients with dizziness, including physiotherapists, chiropractors, occupational therapists, and other clinicians managing vestibular disorders.
It is especially helpful for clinicians who are comfortable treating typical BPPV but feel less confident when findings don’t match textbook patterns.
No. Each of the 7 lessons are self-paced, lasting 2-13 minutes each. You can pause, rewind, and revisit lessons as needed. Many clinicians prefer to return to specific sections when managing complex cases in practice.
Yes. The course is grounded in current research and clinical literature, with references provided to support the concepts and treatment strategies discussed.
Yes. Upon completion, you’ll receive a course certificate, which may be used for continuing education documentation depending on your professional requirements.
Pricing Options
(all prices in CAD)
Regular Price
$38.00
Atypical BPPV of the Posterior Canal - 1 hour online course
Best if you’re focused on atypical BPPV of the posterior canal only
Buy One And Get One At 50% Off
$57.00
- Atypical BPPV of the Posterior Canal - 1 hour online course
- Getting Crystal Clear With Lateral Canal BPPV - 1 hour online course
Ideal if you want a structured approach to complex BPPV
Subscribe And Save
$30.40
Subscribe to our monthly email blast and save 20% on this and all of our online courses
Includes this course + future discounts
Learn a Structured Approach to Atypical BPPV
A subset of patients with posterior canal BPPV present with atypical positional findings, such as negative Dix-Hallpike testing, nystagmus on sitting up, sustained or downbeat torsional nystagmus, or poor response to standard maneuvers leaving clinicians uncertain whether they are dealing with peripheral BPPV, a central disorder, or something else entirely.
Who We Are
Understand why BPPV doesn’t always follow the rules
Too many people live unnecessarily with dizziness and we want help YOU change that.