Lateral Canal Light Cupula: A Case-Based Clinical Reasoning Journey
Lateral canal light cupula can closely mimic lateral canal BPPV, yet it often fails to respond to canalith repositioning or liberatory maneuvers. This case study explores diagnostic features, migraine susceptibility, and clinical reasoning that supports conservative management and an excellent prognosis.
Understanding Light Cupula in the Lateral Canal
Benign paroxysmal positional vertigo (BPPV) is commonly conceptualized as a mechanical disorder driven by free-floating otoconia. In most cases, canalith repositioning maneuvers are highly effective. However, not all gravity-dependent positional nystagmus reflects classic canalithiasis.
Light cupula of the lateral canal represents a cupula-dependent disorder in which the cupula becomes abnormally buoyant relative to the surrounding endolymph. This altered density relationship produces persistent, non-fatiguing, gravity-dependent nystagmus that can closely resemble lateral canal BPPV but behaves very differently. Light cupula is typically a unilateral disorder, affecting one inner ear and producing asymmetric positional responses.
In contrast, cupulolithiasis represents a heavy cupula, most often due to otoconia adhering to the cupula and increasing its density relative to endolymph. This results in sustained gravity-dependent nystagmus driven by cupular deflection in the opposite direction. While both light cupula and cupulolithiasis produce persistent positional nystagmus, their directional patterns and clinical behavior differ, making accurate differentiation essential for management decisions.
This case highlights a presentation consistent with light cupula, emphasizes migraine as a susceptibility factor, and demonstrates why recognizing spontaneous recovery patterns is critical for appropriate management.
For a detailed foundational review of light cupula mechanisms, variants, and clinical patterns, see the companion educational article HERE.
Patient History: Recurrent Positional Vertigo With Inconsistent Response
A 57-year-old female presented with acute positional vertigo. She reported multiple similar episodes over several years, none of which had responded consistently to canalith repositioning or liberatory maneuvers. Despite varied interventions, each episode resolved spontaneously within one to two weeks.
Her medical history was notable for longstanding migraine with episodic headaches and sensory sensitivity. She denied focal neurological symptoms.
Timeline at assessment:
-
Seen five days after symptom onset
-
Estimated 50% improvement at initial visit
-
No vestibular intervention had been performed
Examination Findings
Supine Roll Test
-
Sustained geotropic horizontal nystagmus with head turned to either side
-
More brisk nystagmus and stronger symptoms with left roll
Dix–Hallpike Testing
-
Left Dix–Hallpike provoked symptoms with sustained lateral geotropic nystagmus
-
No torsional or vertical component suggesting posterior canal involvement
Oculomotor examination including smooth pursuit, saccades, gaze-holding, and VOR testing, along with general neurological screening, was unremarkable.
Distinguishing Light Cupula From Typical BPPV and Cupulolithiasis
At first glance, sustained geotropic nystagmus during bilateral roll testing can resemble lateral canal BPPV or, less commonly, cupulolithiasis (heavy cupula). Several features argued against classic canalithiasis:
-
Nystagmus was persistent rather than transient
-
Symptoms were reproducible and non-fatiguing
-
Prior episodes showed inconsistent response to repositioning maneuvers
The presentation also did not fit cupulolithiasis, as lateral canal cupulolithiasis typically produces apogeotropic nystagmus.
Ewald’s laws further support that this presentation does not behave like typical BPPV. For a detailed explanation of how Ewald’s laws apply to vestibular testing click HERE.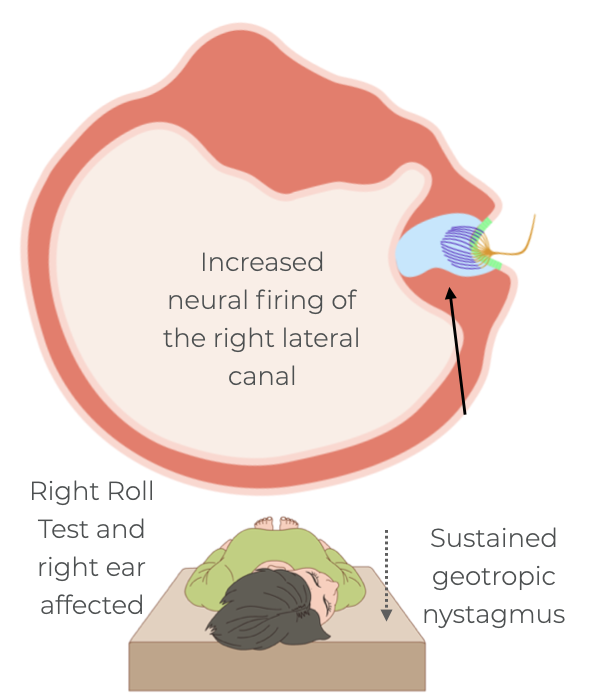
Together, these findings supported a cupula-dependent process consistent with light cupula.
Proposed Mechanisms
Light cupula refers to abnormal buoyancy of the cupula relative to endolymph, producing persistent gravity-dependent deflection.
Proposed mechanisms include:
-
Adherence of degrading otoconia to the cupula, reducing its density (see below)
-
Intrinsic changes in cupular composition
-
Transient alterations in endolymph chemistry
Compared with typical BPPV:
-
Otoconia are not freely mobile
-
Nystagmus is non-fatiguing
-
Mechanical maneuvers often have inconsistent effect
-
Spontaneous resolution is common
Note: There is thought that as otoconia degrade, their density may decrease, potentially becoming less dense than endolymph.
Migraine as a Susceptibility Factor
Migraine is not considered a direct cause of light cupula but likely acts as a predisposing factor. Migraine is increasingly understood as a disorder of sensory gain regulation, ion channel function, and neurovascular control.
The inner ear depends on precise homeostatic regulation of endolymph. In individuals with migraine, relatively small physiologic perturbations may be sufficient to alter cupular buoyancy, helping explain the abrupt onset and rapid spontaneous improvement observed in this case.
Management Considerations
Management of light cupula must account for the underlying mechanism rather than assuming a purely mechanical disorder. Mechanical maneuvers may be beneficial only when light cupula is driven by loosely adherent otoconia that can be detached from the cupula. When abnormal buoyancy reflects intrinsic cupular or endolymphatic changes, these maneuvers are unlikely to produce consistent benefit.
Based on 3D models of the lateral semicircular canal, some clinicians have proposed that lying on the unaffected side may be helpful in select cases. If light cupula is driven by degrading, loosely adherent otoconia that are less dense than endolymph, prolonged positioning on the unaffected side may allow this buoyant material to float upward and away from the undersurface of the cupula, gradually reducing abnormal cupular deflection. While this mechanism remains theoretical, it aligns with observed clinical behavior and the favorable natural history of the condition.
In this case, improvement was already occurring spontaneously, and there was a history of inconsistent response to mechanical maneuvers. Findings were most consistent with a transient physiologic disturbance rather than a persistent mechanical problem. For these reasons management focused on education, reassurance, activity modification, and migraine optimization.
It is also important to acknowledge that light cupula remains an incompletely understood phenomenon. While clinical patterns are increasingly well described, the precise pathophysiology likely varies between individuals, and further research is needed to better define mechanisms and optimal management strategies.
Background reading:
Ichijo H. Cupulopathy: Clinical Features and Pathophysiology. Acta Otolaryngol.
https://pubmed.ncbi.nlm.nih.gov/22986415/
Prognosis
The prognosis is excellent. Typical course includes gradual improvement over days to a couple of weeks and a low risk of chronic vestibular dysfunction. In patients with migraine, recurrence may occur, but episodes are usually self-limited.
Key Clinical Takeaways
-
Persistent geotropic horizontal nystagmus should raise suspicion for a light cupula
-
Migraine may increases vulnerability to transient vestibular disturbances
-
When improvement is already underway, clinical restraint is often the most effective treatment for this condition


