Pupillary Assessment With Infrared Goggles: A Vestibular Therapist’s Guide
Many vestibular clinicians capture eye movements routinely, but what if your infrared goggles were revealing clues about autonomic nervous system function, not just nystagmus?
A chiropractor friend of mine recently sent me a recording of a patient with atypical positional nystagmus, one of those cases where the eye movements do not follow the usual “BPPV patterns.” We worked through the positional findings and landed on a reasonable clinical interpretation and plan.
My friend who shared the recording is an exceptionally sharp clinician, currently working on his PhD, with deep expertise in the autonomic nervous system. What really caught my attention was his notes stating:
Cranial Nerves/Visual: Unremarkable with the exception of pupillary findings.
Pupillary Assessment: Anisocoria present without fixation (infrared goggles); resolves in light. Miotic pupils fail to dilate in darkness. Findings suggestive of diabetic autonomic neuropathy (DAN).
Those findings stopped me, because I had no idea what he was documenting.
Diabetes is incredibly prevalent, and many vestibular clinics now use infrared goggles. If we can observe an autonomic clue during a pupillary assessment with infrared goggles, it raises an important question. Should we be screening for this, or is it simply an interesting rabbit hole?
This blog outlines what I found:
-
What diabetic autonomic neuropathy (DAN) is
-
Why it affects the pupils
-
How it can present clinically
-
What patients might actually complain of
-
And the biggest question. Is there a need for vestibular therapists to screen for this in certain populations, and can it add value to patient care?
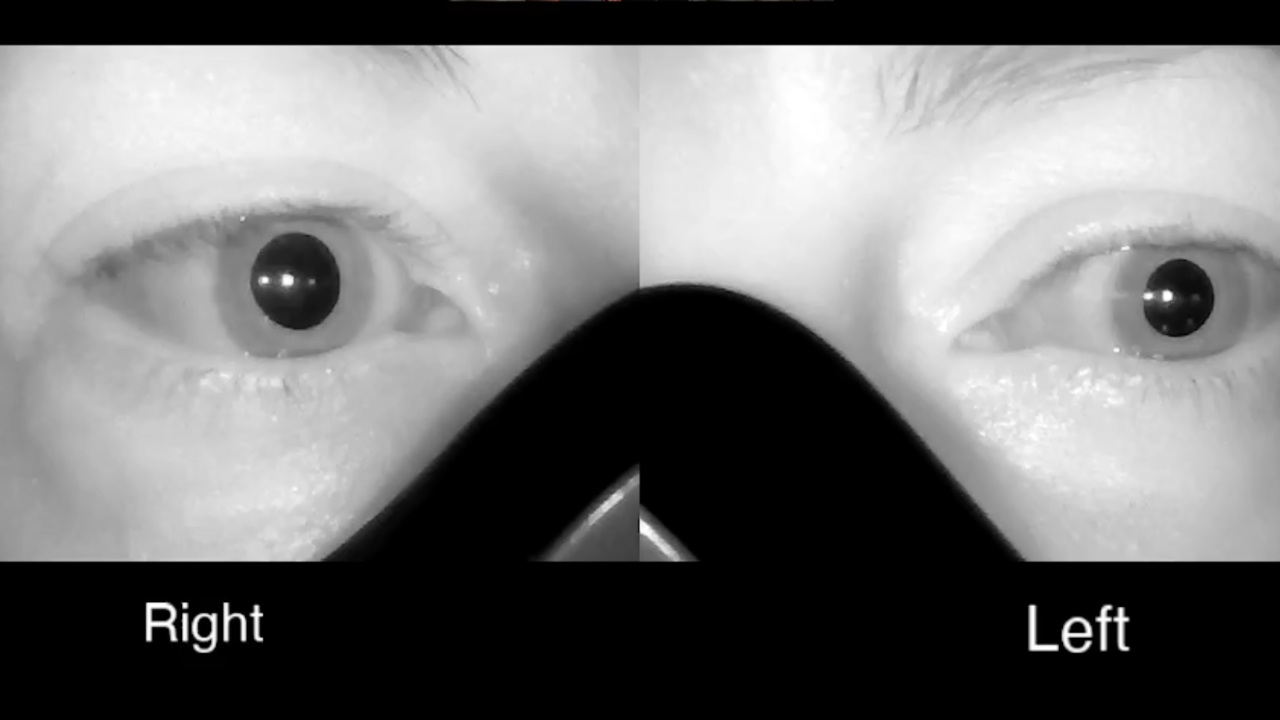
What are we actually seeing?
The pattern described was:
-
Anisocoria without fixation (seen with infrared goggles)
-
Resolves in light
-
Miotic pupils fail to dilate in darkness
This is a lighting dependent clue.
Why anisocoria in the dark matters
Anisocoria simply means unequal pupil sizes. The key is when it appears.
If anisocoria becomes more obvious in darkness, it often suggests impaired dilation, because both pupils should dilate in the dark. If one pupil does not, it stays smaller and the difference becomes more noticeable.
Miotic pupils that do not dilate
If pupils are small and fail to dilate normally in darkness, that points toward reduced sympathetic drive, since the sympathetic system is responsible for dilation.
Why pupillary assessment with infrared goggles matters
Most clinics do not have true darkness. Even dim lighting can influence pupil size, and fixation can also change pupil behaviour.
This is where a pupillary assessment with infrared goggles becomes so useful. Infrared goggles allow you to observe pupils in functional darkness while still seeing them clearly. They let you assess pupil behaviour in the exact environment where dilation problems show up.
With infrared goggles you can:
-
Observe pupil behaviour in darkness
-
Detect subtle anisocoria that only appears when dilation is required
-
Reduce fixation effects
-
Observe dynamic behaviour, not just size but the quality of dilation
Diabetic autonomic neuropathy (DAN) and why diabetes can affect pupil size
Diabetes can affect the autonomic nervous system, not just peripheral sensation and motor function. Autonomic involvement may affect regulation of blood pressure and heart rate, gastrointestinal motility, sweating and thermoregulation, bladder function, and pupillary responses.
The pupil is autonomic
Pupil size is controlled by:
-
Parasympathetic control which constricts the pupil in light
-
Sympathetic control which dilates the pupil in darkness
In diabetic autonomic neuropathy, sympathetic dysfunction can reduce dilation, leading to miotic pupils, sluggish or incomplete dilation, and sometimes anisocoria in darkness.
Is this an early sign of diabetes?
Most often, this is a later or chronic finding.
Pupillary findings consistent with diabetic autonomic neuropathy are more commonly seen after diabetes has been present for years, particularly if glycemic control has been inconsistent. Sometimes it appears early, but that may reflect years of undiagnosed diabetes, prolonged periods of high A1C, or additional risk factors accelerating neuropathy. So if you see this and diabetes is in the history, it may suggest autonomic involvement is already established.
Further reading:
-
American Diabetes Association. Standards of Care in Diabetes: https://diabetesjournals.org/care
What would a patient complain of?
Often, nothing pupil specific. This is frequently a sign, not a symptom.
If they do complain, it is usually low light visual issues:
-
I cannot see as well at night
-
I hate driving at night
-
Dim restaurants are hard to see in
-
It takes longer to adjust when I go into a dark room
Some may also feel more unsteady in darker environments, which is relevant in vestibular rehab. Less visual input means more reliance on vestibular and somatosensory systems.
Functionally, if broader autonomic involvement is present, they may also report:
-
Lightheadedness on standing
-
Exercise intolerance
-
Heat intolerance or reduced sweating
What about concussion and migraine?
Concussion and migraine are common in vestibular practice, and both can involve autonomic dysregulation.
Concussion
Post concussion autonomic features can include exercise intolerance, orthostatic symptoms, fatigue and poor recovery tolerance, and sleep disruption.
From a pupil standpoint, concussion can be associated with:
-
Variable pupil size over time
-
Altered pupillary light reflex dynamics such as sluggishness or asymmetry
-
Photophobia
However, the specific pattern of miotic pupils that fail to dilate in darkness is not a classic concussion signature. If you see it during a pupillary assessment with infrared goggles, it is worth thinking beyond concussion alone.
Migraine and vestibular migraine
Migraine is often autonomic heavy, with symptoms like nausea, flushing or pallor, sweating changes, lightheadedness, and motion sensitivity. Migraine can involve transient pupil irregularities, but these are often variable rather than a consistent fixed pattern of miosis with dilation failure.
Comorbidity matters
Patients can have:
-
Concussion symptoms and diabetes
-
Vestibular migraine and diabetes
-
Migraine physiology and orthostatic intolerance
-
BPPV with broader autonomic dysregulation
So an autonomic clue does not necessarily explain everything. It may simply reveal another layer of the case.
Important: This pupil pattern is not diabetes specific
This finding must be interpreted in context. Several conditions can mimic a similar pupillary pattern, and some can be acute and urgent.
Other conditions that can mimic this pattern
Horner syndrome
Horner syndrome may include miosis, ptosis, and sometimes facial anhidrosis. Anisocoria often becomes more obvious in the dark due to dilation failure.
One important cause of acute Horner syndrome is carotid artery dissection.
Further reading:
-
Horner syndrome overview: https://www.ncbi.nlm.nih.gov/books/NBK500000/
-
Carotid artery dissection overview: https://www.ncbi.nlm.nih.gov/books/NBK441835/
Medication effects or topical exposure
Pupil findings can be influenced by:
-
Opioids
-
Clonidine
-
Ophthalmic drops such as pilocarpine
-
Accidental medication contact even in one eye
Age related small pupils
Older adults may naturally have smaller pupils and reduced dilation, which can mimic autonomic findings.
Other autonomic neuropathies
Other conditions can affect autonomic pupil function, including Parkinson’s disease spectrum disorders, multiple system atrophy, and autoimmune autonomic neuropathies.
So should vestibular therapists screen this and send it to the primary care provider?
Yes, with the right framing.
Vestibular therapists are not diagnosing diabetic autonomic neuropathy, but we can absolutely observe, document, and communicate clinically relevant findings. If you notice miotic pupils, poor dilation in darkness, or anisocoria that changes with lighting during a pupillary assessment with infrared goggles, it is reasonable to document it and recommend follow up.
What I would do in clinic
Document the observation, not the diagnosis.
Example: Pupils appeared miotic in infrared goggles with limited dilation response in darkness. Mild anisocoria noted in darkness which reduced in light.
Check for supporting features:
-
Ptosis
-
New headache or neck pain
-
Other neurological symptoms
Ask targeted questions:
-
Diabetes or prediabetes history
-
Neuropathy symptoms
-
Orthostatic symptoms
-
Changes in sweating, heat tolerance, gastrointestinal function, or bladder function
Consider orthostatic vitals if the story fits.
Communicate with the primary care provider. A short, non-alarmist note can help guide appropriate follow up.
Take home message
Infrared goggles can reveal more than nystagmus. In some patients, a pupillary assessment with infrared goggles can also reveal a pattern of:
-
Miotic pupils
-
Poor dilation in darkness
-
Anisocoria without fixation
This may be consistent with diabetic autonomic neuropathy, but it is not specific to diabetes and must be interpreted in clinical context.
Observe it. Document it. Interpret it carefully. Remember comorbidity is common. Communicate appropriately.
Final thought. Screening vs rabbit hole
Should every vestibular therapist screen this on every patient? Probably not.
But if you already use infrared goggles and you are working with patients who have diabetes, metabolic risk factors, or symptoms suggesting orthostatic intolerance, this observation may add value. Not by giving you a diagnosis, but by helping you recognize when dizziness may be multifactorial and worth medical follow up.


