Blog
Lateral Canal Light Cupula: A Case-Based Clinical Reasoning Journey
Lateral canal light cupula can closely mimic lateral canal BPPV, yet it often fails to respond to canalith repositioning or liberatory maneuvers. This case study explores diagnostic features, migraine susceptibility, and clinical reasoning that supports conservative management and an excellent prognosis.
Understanding Light Cupula in the Lateral Canal
Benign paroxysmal positional vertigo (BPPV) is commonly conceptualized as a mechanical disorder driven by free-floating otoconia. In most cases, canalith repositioning maneuvers are highly effective. However, not all gravity-dependent positional nystagmus reflects classic canalithiasis.
Light cupula of the lateral canal represents a cupula-d...
HINTS Plus Test to Differentiate Stroke from Vestibular Neuritis
Have you ever seen a patient with acute dizziness and wondered whether it could be a stroke? You’re not alone. Distinguishing between a central cause such as a posterior circulation stroke and a peripheral cause like vestibular neuritis can be challenging, especially in the emergency setting.
That’s where the HINTS plus test comes in. This powerful bedside tool helps clinicians determine whether acute dizziness is due to a stroke or a vestibular disorder and it’s been shown to outperform early MRI when used correctly.
In this post, we’ll outline what the HINTS plus test is, how to perform each step, how to interpret the findings, and when to use it in practice.
What Is the HINTS Plus Tes...
Postural Crisis (Tumarkin-like phenomenon) After BPPV Treatment
When I first began treating benign paroxysmal positional vertigo (BPPV), I was advised to: “Always keep a hold on the patient after sitting them up.” It was a warning about the potential for dizziness caused by otolith movement (postural crisis after BPPV treatment) or, more often, due to blood pressure changes during the final step of the maneuver.
Over the years, I’ve followed that advice religiously, wrapping both of my arms around the patient’s neck and shoulders, holding them briefly while making small talk and checking how they are doing.
That is, until one time I didn’t.
I had just completed a modified Epley maneuver with a patient. He looked stable, so I stepped back. But about 15...
A Deeper Look at SVINT: A Powerful, Underused Tool in Vestibular Assessment

At North 49, I’ve been incredibly fortunate to learn from many brilliant clinicians throughout my career and I see it as part of my responsibility to share what I’ve learned along the way. My goal is that these blogs are a means of reviewing what I have learned and assist in supporting your journey by offering practical, evidence-based insights.
This blog, however, is a little different.
It’s a summary of a doctoral project by someone I’ve had the honour of working with for several years: Nycole Pataki. Nycole recently relocated from Saskatchewan to Arizona with her family and asked if I’d read her doctoral project. After doing so, I knew this work deserved a broader audience. With her per...
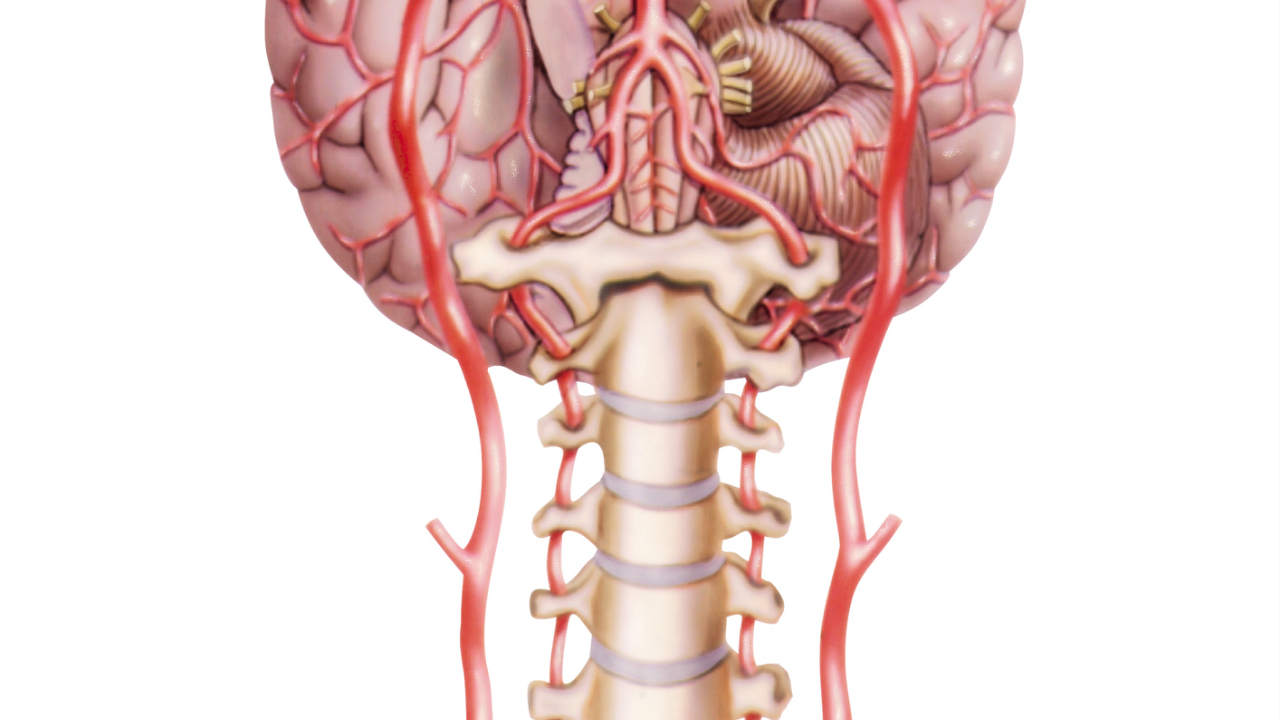
Vestibular Neuritis: A Deeper Dive Into the Pathophysiology
Vestibular neuritis is one of the more common causes of acute vertigo seen in emergency rooms and vestibular therapy clinics alike. It is estimated to account for 3.2 to 9% of all vertigo cases seen in specialized dizziness clinics [1], and has an incidence of approximately 3.5 per 100,000 people per year [2]. While many therapists understand its classic clinical presentation of sudden onset of vertigo/dizziness lasting days, often with nausea, imbalance, and spontaneous nystagmus the underlying pathophysiology deserves a closer look.
The Classic Presentation of Vestibular Neuritis
Vestibular neuritis (most commonly due to a viral infection) typically results in an acute unilateral vestibu...
Vestibular Paroxysmia: What It Is & Why We Should Be Aware of It

In this blog, I want to share something that over the past couple of years has repeatedly come across my path being Vestibular Paroxysmia. I first remembering hearing about it from Dr. Shepard on the Talk Dizzy to Me podcast, then glanced through it on the Bárány Society website, and more recently it came up during the Advanced Vestibular Physical Therapy cohort I was fortunate to be in through the University of Pittsburgh
I’ve come to realize that, although this condition is not common, it’s certainly out there and as clinicians who work with people dealing with dizziness, we need to keep this one in the back of our minds. My approach is: if I see something once, I park it in the back of m...
Gaze Stabilization Exercises: 3 Advanced Progressions

Gaze stabilization exercises, such as X1 and X2 exercises, are essential in vestibular rehabilitation for patients with unilateral vestibular hypofunction (UVH). Standard progressions typically involve increasing the duration, transitioning from a plain to a busy background, adding balance challenges, and advancing to X2 exercises. However, beyond these standard progressions, there are additional strategies that can further enhance a patient's recovery.
In this post, we will review three additional progression options that have proven useful in clinical practice.
Gaze Stabilization Progression #1: Bringing the Target Closer
How to Perform:
Patients perform the X1 gaze stabilization exerci...
The Storage Velocity Mechanism: A Guide for Vestibular Therapists

In an effort to better understand the Storage Velocity Mechanism (SVM) and its clinical significance—something that isn’t talked about much in courses—I decided to dive deeper into what it is, why it matters, and what I should know as a vestibular therapist. Here’s what I found.
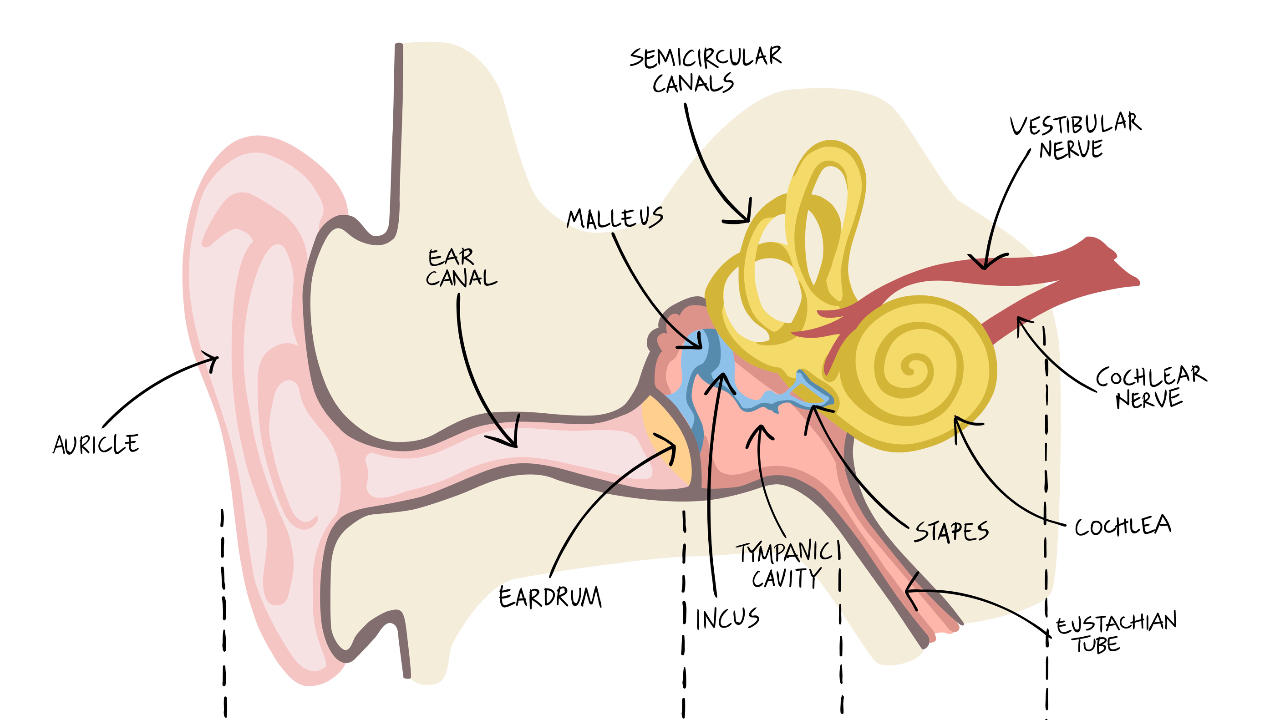
What is the Storage Velocity Mechanism?
As we know, the semicircular canals detect angular acceleration. However, with motion at a steady speed the cupula in the semicircular canal returns to its resting position within 7 seconds. Despite this, we can maintain visual stability during sustained rotations, thanks to the Storage Velocity Mechanism (SVM).
The SVM essentially integrates and "stores" velocity informa...
Understanding Third Window Syndrome (TWS)

As healthcare providers, we occasionally encounter patients with dizziness that does not fit the usual patterns of vestibular disorders. One such condition is Third Window Syndrome (TWS), which most commonly presents as Superior Semicircular Canal Dehiscence (SSCD). There are other presentations of TWS aside from SSCD and TWS itself was first described by Minor in 1998.
In this blog, we will cover what TWS is, its causes, symptoms, triggers, diagnosis, and treatment options.
What is Third Window Syndrome?
Third Window Syndrome (TWS) encompasses a group of inner ear disorders characterized by an abnormal opening or thinning in the bony structures of the inner ear. The most well-known form...
Exploring the Skull Vibration Induced Nystagmus Test (SVINT)

We’re excited to share an assessment technique that has significantly enhanced our ability to evaluate patients with vestibular hypofunction: the Skull Vibration Induced Nystagmus Test (SVINT). After hearing about it a few times over the past few years, we decided to investigate further and are glad we did. Given our access to infrared goggles, implementing SVINT was quite affordable since portable handheld massage devices can be picked up at places like Walmart.
Clinically, the test has helped us pick up vestibular hypofunctions when our other battery of tests such as looking for gaze evoked nystagmus, head impulse test, head shaking nystagmus test, and dynamic visual acuity tests were unr...


