Vestibular Neuritis: A Deeper Dive Into the Pathophysiology
Vestibular neuritis is one of the more common causes of acute vertigo seen in emergency rooms and vestibular therapy clinics alike. It is estimated to account for 3.2 to 9% of all vertigo cases seen in specialized dizziness clinics [1], and has an incidence of approximately 3.5 per 100,000 people per year [2]. While many therapists understand its classic clinical presentation of sudden onset of vertigo/dizziness lasting days, often with nausea, imbalance, and spontaneous nystagmus the underlying pathophysiology deserves a closer look.
The Classic Presentation of Vestibular Neuritis
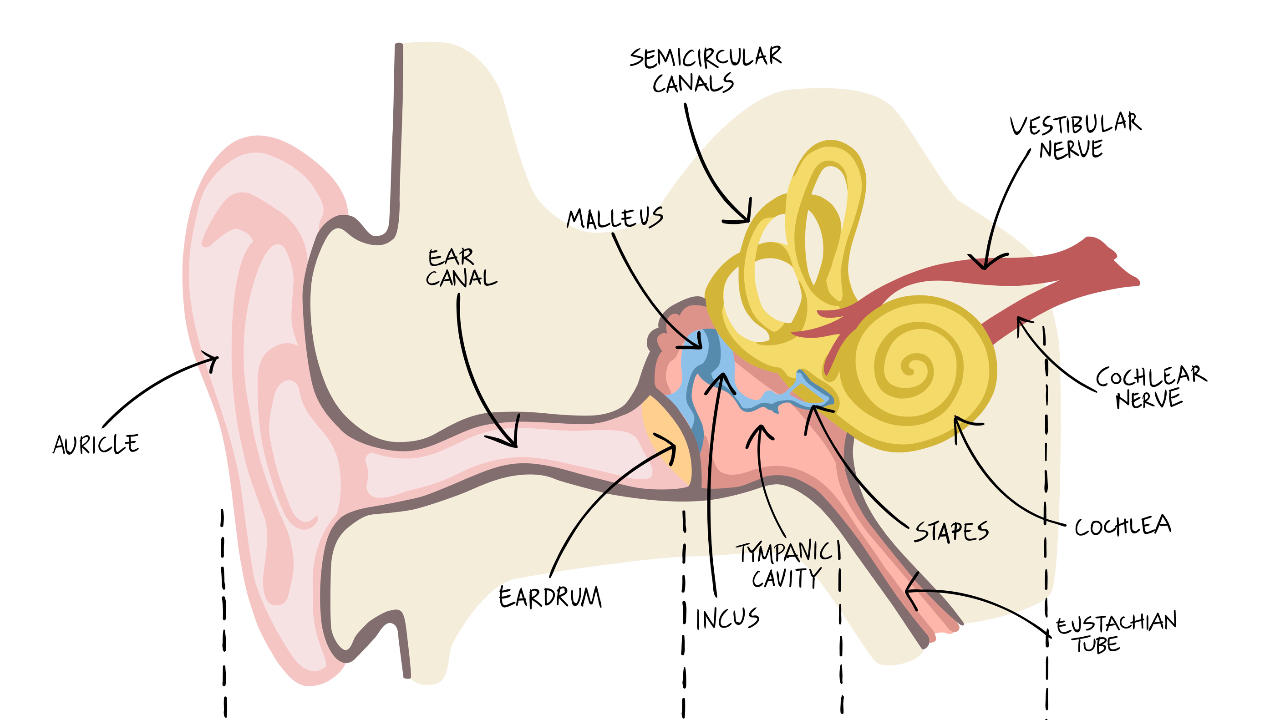
Vestibular neuritis (most commonly due to a viral infection) typically results in an acute unilateral vestibular loss that affects the superior branch of the vestibular nerve more than the inferior branch. This upper branch innervates the anterior and horizontal semicircular canals, along with the utricle. When this pathway becomes inflamed, it creates an imbalance of neural firing between the two ears, leading to constant vertigo/dizziness and spontaneous horizontal-torsional nystagmus, especially in the first 24–72 hours.
To see examples of nystagmus from a unilateral vestibular loss click HERE.
As swelling subsides and the brain begins central compensation, the nystagmus becomes intermittent and less intense, and the patient gradually reports improved stability and resolution of symptoms.
But here’s the part that often goes unexamined—how does an infection even get to the vestibular nerve in the first place?
A Virus With Staying Power: Herpes Zoster
A leading theory is that vestibular neuritis is most often caused by reactivation of herpes simplex virus type 1 (HSV-1), the same virus responsible for cold sores [3]. Following primary infection, HSV-1 becomes latent and resides in cranial nerve ganglia, including the vestibular (Scarpa’s) ganglion within the temporal bone. Studies have detected HSV-1 DNA in the vestibular nerve of individuals with a history of vestibular neuritis [4]. HSV-1 is notably elusive, capable of invading a wide range of tissues and, in some cases, even crossing the blood-brain barrier to cause encephalitis.
Once inside us, the virus never truly leaves. Instead, it lies dormant—often in the trigeminal or vestibular ganglia. Reactivation can occur years or decades later due to triggers like stress, fatigue, immune suppression, or systemic illness.
It’s worth noting that cold sores affect up to 67% of the global population by age 50 [5], so having HSV-1 isn’t rare. What is rarer is the reactivation that leads to inflammation specifically in the vestibular nerve. While people can have recurrent cold sores, recurrent vestibular neuritis is uncommon. This may be due to the immune system developing a localized, more robust response in that region after the first attack, or possibly because not all nerve ganglia have the same viral load or susceptibility.
Pathoanatomy and Inflammation
Once reactivated, HSV-1 travels down the vestibular nerve, causing local inflammation and demyelination, disrupting signal conduction. This disconnect leads to a mismatch in vestibular input between sides and results in the hallmark vertigo/dizziness, spontaneous nystagmus, and imbalance.
Most commonly, the superior branch of the vestibular nerve is affected. This may be because the bony canal through which it passes is narrower, making it more susceptible to compression and ischemia when swollen.
Prognosis and Central Compensation
The good news is the prognosis is generally favourable. Most patients improve significantly within a few weeks, although balance issues and visual motion sensitivity can linger for months—particularly when compensation is incomplete. If inflammation causes neurapraxia (a temporary loss of function due to demyelination or compression without axon loss), the vestibular nerve can fully recover over time, typically within weeks to months.
Central compensation also plays a key role in recovery. The brain adapts by recalibrating sensory input—relying more on vision and proprioception while re-weighting vestibular signals. However, this compensation process can be delayed in older adults or in individuals who reduce their activity levels after the episode. Early movement and vestibular rehabilitation can help accelerate both peripheral and central recovery.
Role of Gaze Stabilization Exercises in Recovery
This is where vestibular rehabilitation therapy (VRT), especially gaze stabilization exercises, becomes critical. These exercises, such as X1 and X2 viewing, aim to retrain the vestibular system to stabilize gaze with head movement.
Early and tailored vestibular rehabilitation can significantly speed up the recovery process and reduce long-term deficits in function [7].
To see our favourite progressions for gaze stabilization exercises click HERE.
Final Thoughts
Understanding the pathophysiology of vestibular neuritis helps us assess and treat it more effectively. While its viral origin may seem mysterious given the inner ear’s enclosed structure, recognizing the role of HSV-1, nerve inflammation, and central compensation clarifies why symptoms evolve the way they do—and why vestibular therapy plays such a key role in recovery.
Next time you see a patient with acute vestibular loss, consider the journey of that virus from a cold sore in youth to inflammation in the inner ear decades later. And keep emphasizing those gaze stabilization exercises because motion, not rest, is the path to recovery.
If you would like to see more vestibular therapy educational opportunities, check out our website and YouTube channel.


