Blog
Lateral Canal Light Cupula: A Case-Based Clinical Reasoning Journey
Lateral canal light cupula can closely mimic lateral canal BPPV, yet it often fails to respond to canalith repositioning or liberatory maneuvers. This case study explores diagnostic features, migraine susceptibility, and clinical reasoning that supports conservative management and an excellent prognosis.
Understanding Light Cupula in the Lateral Canal
Benign paroxysmal positional vertigo (BPPV) is commonly conceptualized as a mechanical disorder driven by free-floating otoconia. In most cases, canalith repositioning maneuvers are highly effective. However, not all gravity-dependent positional nystagmus reflects classic canalithiasis.
Light cupula of the lateral canal represents a cupula-d...
HINTS Plus Test to Differentiate Stroke from Vestibular Neuritis
Have you ever seen a patient with acute dizziness and wondered whether it could be a stroke? You’re not alone. Distinguishing between a central cause such as a posterior circulation stroke and a peripheral cause like vestibular neuritis can be challenging, especially in the emergency setting.
That’s where the HINTS plus test comes in. This powerful bedside tool helps clinicians determine whether acute dizziness is due to a stroke or a vestibular disorder and it’s been shown to outperform early MRI when used correctly.
In this post, we’ll outline what the HINTS plus test is, how to perform each step, how to interpret the findings, and when to use it in practice.
What Is the HINTS Plus Tes...
Acute Dizziness Management: Vestibular Regulation Tools

As vestibular therapists, we’re well-versed in adaptation, habituation, and substitution. These principles are the foundation of vestibular rehabilitation and are vital for long-term recovery. However, there seems to have been less emphasis in our field on equipping patients with acute dizziness management strategies, the tools they can use to calm symptoms when they spike, whether after doing their exercises or when caught in a visually or motion-rich environment.
That gap inspired this post. Over the years at North 49, I’ve found that teaching vestibular regulation techniques can empower patients to manage dizziness in real time, giving them confidence and control while supporting long-te...
Vestibular Forensics: The Vestibular System and Spatial Disorientation
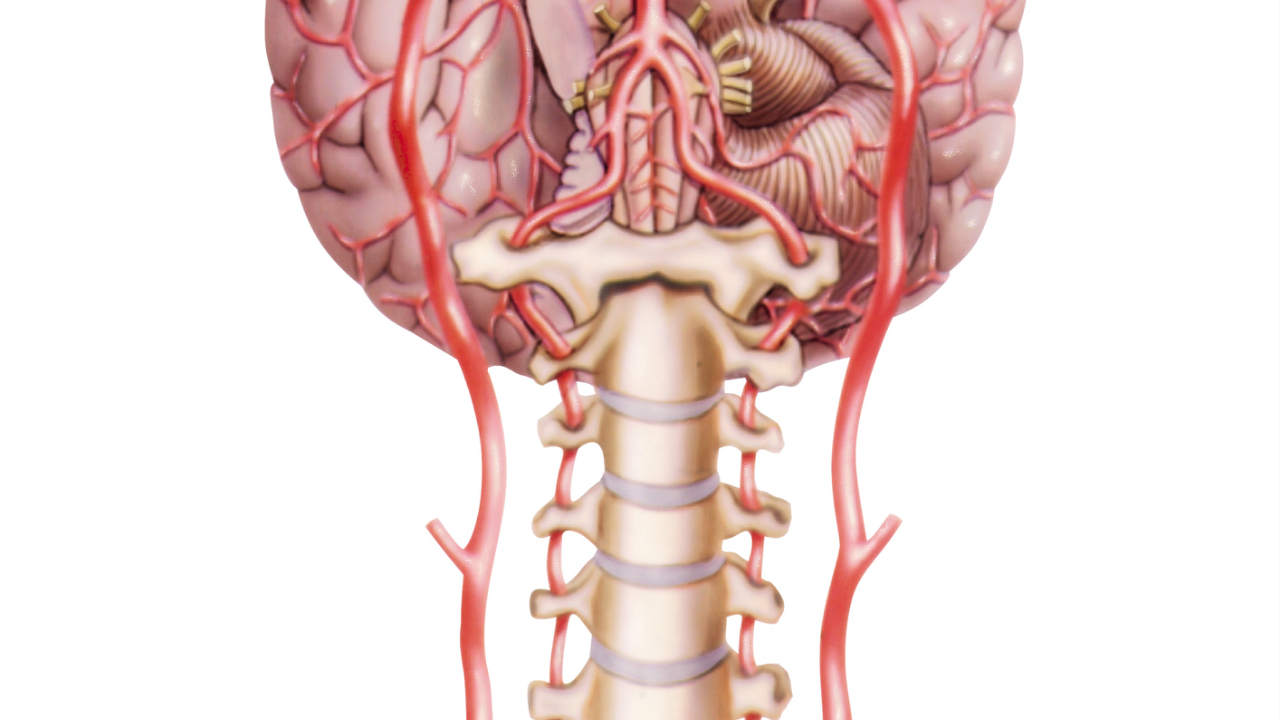
Most of us do not think about the vestibular system until something goes wrong. Yet this hidden sensory system works constantly in the background, keeping us upright, stabilizing our vision when we move our head, and even helping regulate blood pressure when we change posture. However, when vestibular input is impaired, the consequences can be profound: dizziness, disorientation, blurred vision, or even catastrophic accidents in aviation and spaceflight.
Understanding the vestibular system and spatial disorientation not only improves clinical care, but also explains why pilots crash, why astronauts get sick, and why patients describe feeling like they do.
The Vestibular System and Its Role...
Pediatric Vestibular Assessment: A Guide for Clinicians

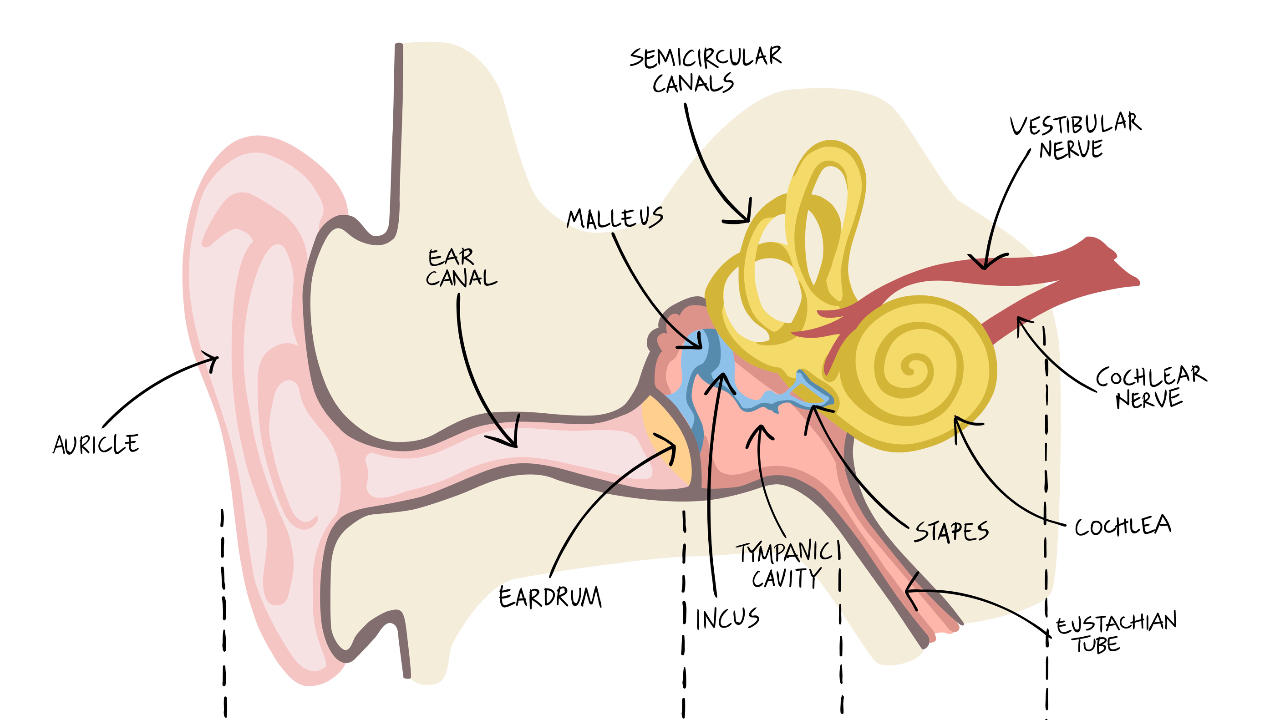
Why Pediatric Vestibular Assessment Matters
Pediatric vestibular assessment is an often-overlooked area in clinical practice. Yet research shows that nearly 50% of children with hearing loss have some degree of vestibular dysfunction (Cushing et al., 2013; Verbecque et al., 2017). Risk is higher in children with:
-
Severe hearing loss (>66 dB)
-
Structural inner ear anomalies (e.g., enlarged vestibular aqueduct)
-
Congenital cytomegalovirus
-
Usher syndrome type 1
-
Meningitis or temporal bone fracture
-
Ototoxic medication exposure
Undetected vestibular loss in children can lead to gross motor delays, poor postural control, academic challenges, and limited partici...
Postural Crisis (Tumarkin-like phenomenon) After BPPV Treatment
When I first began treating benign paroxysmal positional vertigo (BPPV), I was advised to: “Always keep a hold on the patient after sitting them up.” It was a warning about the potential for dizziness caused by otolith movement (postural crisis after BPPV treatment) or, more often, due to blood pressure changes during the final step of the maneuver.
Over the years, I’ve followed that advice religiously, wrapping both of my arms around the patient’s neck and shoulders, holding them briefly while making small talk and checking how they are doing.
That is, until one time I didn’t.
I had just completed a modified Epley maneuver with a patient. He looked stable, so I stepped back. But about 15...
Vestibular Neuritis: A Deeper Dive Into the Pathophysiology
Vestibular neuritis is one of the more common causes of acute vertigo seen in emergency rooms and vestibular therapy clinics alike. It is estimated to account for 3.2 to 9% of all vertigo cases seen in specialized dizziness clinics [1], and has an incidence of approximately 3.5 per 100,000 people per year [2]. While many therapists understand its classic clinical presentation of sudden onset of vertigo/dizziness lasting days, often with nausea, imbalance, and spontaneous nystagmus the underlying pathophysiology deserves a closer look.
The Classic Presentation of Vestibular Neuritis
Vestibular neuritis (most commonly due to a viral infection) typically results in an acute unilateral vestibu...
Vestibular Paroxysmia: What It Is & Why We Should Be Aware of It

In this blog, I want to share something that over the past couple of years has repeatedly come across my path being Vestibular Paroxysmia. I first remembering hearing about it from Dr. Shepard on the Talk Dizzy to Me podcast, then glanced through it on the Bárány Society website, and more recently it came up during the Advanced Vestibular Physical Therapy cohort I was fortunate to be in through the University of Pittsburgh
I’ve come to realize that, although this condition is not common, it’s certainly out there and as clinicians who work with people dealing with dizziness, we need to keep this one in the back of our minds. My approach is: if I see something once, I park it in the back of m...
Gaze Stabilization Exercises: 3 Advanced Progressions

Gaze stabilization exercises, such as X1 and X2 exercises, are essential in vestibular rehabilitation for patients with unilateral vestibular hypofunction (UVH). Standard progressions typically involve increasing the duration, transitioning from a plain to a busy background, adding balance challenges, and advancing to X2 exercises. However, beyond these standard progressions, there are additional strategies that can further enhance a patient's recovery.
In this post, we will review three additional progression options that have proven useful in clinical practice.
Gaze Stabilization Progression #1: Bringing the Target Closer
How to Perform:
Patients perform the X1 gaze stabilization exerci...
PPPD Demystified: Understanding Persistent Postural Perceptual Dizziness

Persistent Postural Perceptual Dizziness (PPPD or 3PD) is a chronic functional vestibular condition that can be a challenge to manage. While it isn’t caused by structural damage or psychiatric disorders, it’s one of the most common reasons people experience long-term dizziness. This condition is especially prevalent in specialized dizziness centers, where understanding PPPD can make a big difference in patient care. Let’s take a closer look at its symptoms, history, and what healthcare providers need to know. We hope that in sharing what we have found, this helps you better understand this challenging condition and improve patient outcomes.
What Does PPPD Look Like?
Patients with PPPD ofte...


